Dr. Ha's Article on Envision Magazine
Everyone develops presbyopia or age-related farsightedness. It starts somewhere around age 40 for emmetropes, the mid-to-late 30s for hyperopes and the mid-40s-plus for myopes. It's the classic ocular sign - the first reminder of aging that a person experiences, besides the crow's feet they "see". Almost overnight, your arms aren't long enough to hold the menu, phone or book far enough away to see clearly. Other symptoms include squinting, headaches, eyestrain and fatigue, that accompany prolonged near activities. The experience can be quite emotional for some presbyopes and is often accompanied by a period of denial, with many people feeling depressed and frustrated with failing eyes that have supported them for nearly four decades.
Among the more than two billion people with presbyopia worldwide', it's estimated that the global unmet need for presbyopia correction is 45 per cent2. This represents an enormous market for the eyecare community and reflects the paradigm shift that is happening in the world of presbyopia. Is it any wonder industry partners are pouring money into R&D to create products for this category of patients? Methods of correcting presbyopia are progressing with greater opportunities for eyecare practitioners (ECPs) and more choices for patients than ever before. But to date, none of them is perfect.
SPECTACLES AND CONTACT LENSES
By far the most frequently offered option remains reading glasses or spectacles with lined bifocals or trifocals and progressive addition lenses. More recently, however, the multifocal contact lens market share has grown; ECPs are prescribing them more frequently, due to technological advances in lens design, materials and manufacturing methods, as well as the availability of various multifocal contact lens options (distance-centred, near-centred, toric, scleral, aspheric, hybrid, extended depth of focus (EDOF), and nasally decentered optics). As well, practitioners are more confident in prescribing and fitting them.
ELECTIVE SURGICAL PROCEDURES
1. Presbyopic laser refractive surgery: While there is a gain in the presbyope's near vision, monovision excimer laser ablation (laser in situ keratomileusis or LASIK, photorefractive keratectomy or PRK, femtosecond lenticule extraction or FLEx, small incision lenticule extraction or SMILE, Intralase Sub-Bowman's Keratomileusis or SBK) typically compromises binocular vision and sometimes even distance vision.
2. The presbyopic-correcting (PC) intraocular lens (IOL): This is geared more to presbyopes who want to lessen or eliminate their dependency on glasses. The advancement of this teknologu over the past 10-15 years has been revolutionary with each subsequent IOL model taking a giant step forward from the previous generation. The challenges with the former models have always been intermediate vision and dysphotopsia: glare and halos, especially at night. The latest trifocal diffractive IOL (PanOptif from Alcon) improves intermediate vision by providing a third focus, while the extended depth of focus or EDOF IOL (TECNIS Symphony' from Johnson & Johnson Vision, low-add Vivity® from Alcon) creates an elongated focal point to increase the range of near vision, with both showing less visual disturbance than their predecessors.
The innovations are continuing with:
- the next generation refractive monofocal IOL with higher-order aspheric design, that improves intermediate vision (TECNIS Eyhance®) and the EDOF-multifocal hybrid (TECNIS Synergy), both from Johnson & Jonhson Vision
- the monofocal IOL with 1-D of EDOF for those who are not candidates for diffractive trifocal IOLs (RayOne EMV® from Rayner Global)
- the Light Adjustable Intraocular lens (LAL") from RXSight® that offers near vision correction using EDOF technology and allows post-operative IOL spherical/ cylindrical power adjustments to suit the person's visual needs.
" In the coming decade, if PC IOL technology continues as it is now and there is an adjustable EDOF lens in the marketplace, refractive lens exchange or clear lens extraction may become the norm for defeating Father Time"
3. Keratophakia or corneal inlays: These are permanent-yet-reversible implants that are surgically inserted into the corneal stromal tissue of the non-dominant eye to help manage presbyopia by increasing the eye's depth of focus at near. They may be combined with LASIK in eyes that have refractive error. Compared to monovision correction, there is usually a five-to-six-line gain in near vision with one or no lines lost in distance vision with inlays, versus only a one-line gain in near vision for every line lost in distance vision with monovision3. Side effects include decreased contrast sensitivity, decreased night vision, compromised distance vision, and the long-term risk for interface haze development between the cornea and the hydrogel material.
Several corneal inlays were introduced to the marketplace but the adoption rate by both surgeons and patients has been slow and not widespread. Any momentum that inlays experienced was dampened by the FDA recall of the Raindrop' inlay from ReVision Optics in 2019. The negative ripple effect left only one corneal inlay currently on the market - the small aperture KAMRA® inlay by AcuFocus. With emerging treatment options such as pupillary miotics (below) becoming more available, the future of corneal inlays looks poor, unless newer materials with enhanced biocompatibility are developed. At the time of writing, clinical trials are underway for the refractive Presbia Flexivue Microlens-from PresbiBio that is similar to multifocal contact lenses and IOL, LLC and allogenic inlays.
"The perfect presbyopia-correcting eye drop should provide improvement in a range of uncorrected vision at near with minimal compromise to distance vision and restore accommodation."
PRESBYOPIA-CORRECTING EYE DROPS
The newest game-changing presbyopia management tool could be pharmaceutical agents - miotic-based and lens-restoration eye drops. The perfect presbyopia-correcting eye drop should provide improvement in a range of uncorrected vision at near with minimal compromise to distance vision and restore accommodation. The drop should also be comfortable on instillation, fast-acting and long-lasting with excellent safety and minimal adverse effect profiles.
1. Miotic-based drops allow the pupil or aperture to constrict and create a pinhole effect that increases the eye's depth of focus. AGN-190584 (Vuity: 1.25% Pilocarpine HC1) by Allergan, an AbbVie company, has already been approved and is on the market.
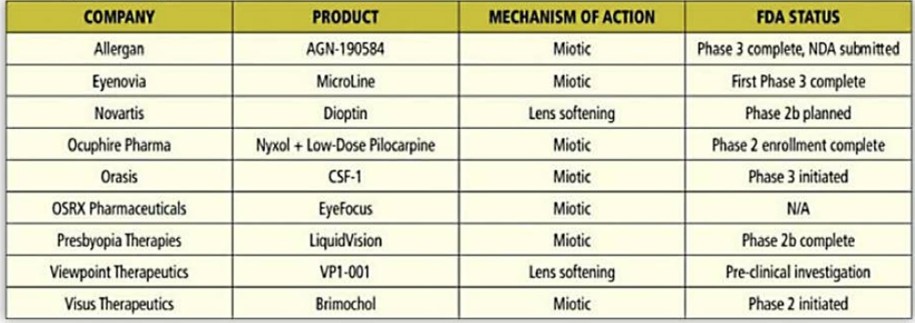
Presbyopia drop overview
2. Lens restoration eye drops, on the other hand, purport to restore accommodation at the root of presbyopia by softening the lens proteins (Novartis - Dioptin) to restore elasticity or by stabilizing the lens protein (Viewpoint Therapeutics VP1 -001 ) to prevent stiffening.
Presbyopia-correcting eye drops are not to be taken as an absolute replacement for reading glasses, contact lenses or surgery but as a supplement to these and other modalities. At the time of writing, there are nine presbyopia-correcting eye drop solutions in various phases of clinical trials (Table 1)4 and many are expected to receive regulatory approval in the near future. For the millions of presbyopes in Canada and the U.S., the prospect of a new treatment strategy is most welcome news.
"The biggest unmet need, and a massive opportunity for the eyecare industry, is the "emmetropes", not just the natural ones but also those without any refractive errors, because they have had refractive surgery or wear contact lenses or glasses for distance, who are now experiencing presbyopia."
EDUCATION & MANAGEMENT
It is important to take a proactive approach and begin a discussion about presbyopia based on the expected onset of the condition. The biggest unmet need, and a massive opportunity for the eyecare industry, is the "emmetropes”, not just the natural ones but also those without any refractive errors, because they have had refractive surgery or wear contact lenses or glasses for distance, who are now experiencing presbyopia.
There exist similarities yet distinct differences between the different categories of refractive errors and presbyopic treatment options. Knowing which innovations are available and which are in the pipeline can guide the conversation about the best-individualized options for the patient, especially if you take into account their questions and concerns and adjust, establish and manage their expectations. bu rakamlı olanlar cok içerde, on un için böyle yapıyom..
1. The natural emmetrope is a challenging category. If not already wearing reading glasses, they are often seen when coming in for their first eye exam while in the midst of presbyopia. They have no idea what is happening to them because they have never required any type of refractive correction or worn/placed anything on their nose/face/eyes. Their biggest concern is, "I can't see up close Education and adjusting/ setting their expectations are key to managing their journey as their eyes progressively change over the coming decades. Despite laying out their different options, including the new technologies coming through the pipeline, they are often the hardest to convince that their vision will not return to a pre-presbyopia state. They are usually averse to the risks associated with surgical interventions and difficult to fit with glasses as well. If both the natural and pseudo-emmetropes understand and accept that there is currently no perfect solution for them, then the present-day solution with a multifocal contact lens in one eye, along with presbyopia-correcting pharmaceutical agents, works nicely for them.
2. The hyperope, when compared to the emmetrope and myope, is the easiest group, especially the mild-to-moderate latent ones who present in their mid-to-late-30s with blur at near and without symptoms at a distance. As an added bonus, placing anything on them will improve their distance vision, which they love.
Depending on whether or not they want glasses, the discussion can easily turn to contact lenses, surgical options, and soon-to-be-introduced pharmaceuticals. The only proviso is lens handling, as the presbyopia increases and hyperopes will always need an auxiliary pair of glasses
3. Myopes are an interesting lot and require a lot of hand-holding to successfully navigate their presbyopia. They present ECPs with a different set of challenges, depending on what their current treatment modality is, what they want to fit their current lifestyle and the treatment option selected. The most difficult challenge is explaining to myopes why they can't see up close with their distance correction but can see up close when they take off their glasses/contact lenses. The idea is often too abstract for them to comprehend.
Myopes who just want to transition into progressive add (PAL) lenses and have no interest in refractive surgery or contact lenses, need to be educated that there will always be a compromise with PALS at near. For low-to-moderate myopes engaged in visually demanding near activities, a recommendation to remove their glasses is the best option. For those already in contact lenses, the options would include reading glasses over contact lenses as needed for near, monovision or multifocal contact lenses and presbyopia-correcting eye drops. For those in distance correction who are considering an elective refractive procedure, a thorough discussion about presbyopia and the impact after surgery on close-up vision and the eventual need for near correction is required. In all scenarios, myopes must be aware that all the current presbyopic solutions are compromises.
"For ECPs, creating and nurturing relationships with these patients is paramount in building trust and restoring patients' peace of mind as they face the optical consequences of advancing age."
THE OPPORTUNITY FOR ECPS
For patients who enjoyed 20/20 vision most of their lives, a diagnosis of presbyopia can be disturbing and disruptive. For ECPs, creating and nurturing relationships with these patients is paramount in building trust and restoring patients' peace of mind as they face the optical consequences of advancing age.
The treatment of presbyopia is highly individual and must be considered on a case-by-case basis, taking into account the starting refractive error, level of presbyopia, lifestyle and compliance with the chosen treatment and its possible after-effects. The ultimate objective of presbyopia treatment is to address the biggest concern, which is not being able to see up close. ECPs can play a key role in helping their patients achieve that objective. Patient communication, counselling and hand-holding are vital tools in an ECP's armamentarium, as are the treatment techniques chosen to address each presbyope's individual case.

